13year old male patient
"This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment"
13 year old boy came to our opd with history of yellowish discoloration of eyes ,yellow colored urine since 9 days .
HOPI:
A13 years male patient - he came with history of yellowish discoloration of eyes since 9 days .
One episode of bilious vomiting .
He also complaints of yellow colour urine and dark coloured stools since 9days
PAST history :
He is the youngest of all .
He was born out of normal vaginal delivery with 4kgs birth weight ,cried immediately after birth .
He had jaundice at birth ,that resolved spontaneously .? Physiological jaundice.
He is Immunised as per schedule .
At 8 months of age patient had history of altered bowel habits - one week of loose stools and one week of normal consistency stools for few days later he was passing loose stools every day for 2-3 months ,during which he became very cachetic .
He got admitted in a hospital ,in the discharge summary - they mentioned as suspected case of celiac disease ,chronic diarrhea ,chronic malabsorption .
During the hospital stay he was given Iv antibiotic and 2FFP transfusions .He recovered in 3 months according to parents .
On further asking parents ,they told he used to have recurrent colds ,cough and fever .He used inhalers for 1 year during winters in childhood . Though he wasn't admitted at any point , and there was no history of pnuemonia.
At 9 years of age - parents noticed neck swelling and they took him to ENT doctor ,later referred to endocrinologist ,where he was diagnosed with hypothyroidism - intial TSH was -150 ,he was started with 150 mcg of thyronorm,later increased to 180 mcg .
patient also gives history of chronic itching over hands and foot since the age of 9 years .
At 12 years of age patient had chicken pox ,resolved over 10 days.
PERSONAL HISTORY
FAMILY HISTORY:
He is a 4th order child ,born out of grade 4 consanguinous marriage
He has 2 elder brothers and one elder sister - who expired at 5 years of age .
His sister was the first child and she was assymoptomatic till 2 years of age ,then she had shortness of breath and was rushed to hospital,where here condition detiorated and got admitted .They were told that she had splenomegaly and Her blood counts were decreasing .She was given multiple blood transfusions every 25 days for one year inspite of that she remained anemic ,she also underwent bone marrow biopsy twice .
According to parents she was given steriods also for one year before death .she never had jaundice or recurrent infections.
.Elder brother is 19 year old and second brother is -16 years old .
Second one had history of fever ,white coloured loose stools at the age of 5 years ,for which they went to nalgonda hospital .He was given some medications and it got resolved .But he was said to have anemia ,and he recovered according to parents with some medications.There was no jaundice and no history of blood transfusion.
On general examination -
He is thin built .
Height -156 cm
Weight - 32kgs
icterus + ,pallor + ,cyanosis -, clubbing - , edema - , lymphadenopathy -.
SYSTEMIC EXAMINATION:
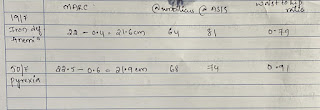
Outside investigations -
There is significant drop in hemoglobin from 8.9 to recent HB -5,leucopenia , thrombocytopenia.
With raised bilirubin - both direct and indirect , normal enzymes .
Urine for bile salts and bile pigments + ve
HB electrophoresis - normal .
Serology for HiV ,HBSag , Hcv was negative
Dengue , Malaria ,widal was negative
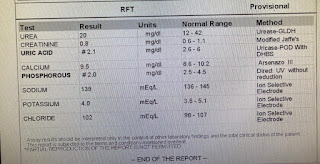
Investigations
Treatment:
Tab- thyronorm-200mcg PO OD
Tab-methylprednisolone 32 mg PO OD
Tab-Atarax-10mg PO OD
Physiocoel lotion-BD
Assessment :
? Spectrum of Autoimmune diseases -
Thyroditis ,? AIHA
Chronic itching of both hands and limbs
? CVID
Plan - repeat CBP with peripheral smear ,LDH ,retic count ,coombs test .
Other routine investigations
Dermatology opinion .











Comments
Post a Comment