Answer: It is due to kindling. Kindling refers to the phenomenon of increasingly severe withdrawal symptoms, including an increased risk of seizures, that occurs as a result of repeated withdrawal from alcohol or other sedative–hypnotics with related modes of action.
Answer: Thiamine replacement is the primary treatment for WKS in order to reverse mental status changes and prevent further disease progression. Parenteral thiamine is used in the acute treatment of Wernicke's since intestinal absorption of thiamine may be impaired, as in the case of alcoholics.
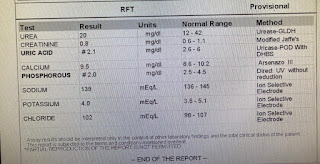
Answer: kidney injury - ↓ synthesis of erythropoietin →↓ stimulation of RBC production → normocytic, normochromic anemia. The chronic alcoholism leads to the fewer mature RBCs which I turn leads to normocytic anemia
Answer: Excessive alcohol can cause nutritional deficiencies and alcohol toxicity. These in turn can cause poor nutrition leading to poor wound healing and problems with the nerves (neuropathy). When the sensory nerves in the foot stop working, the foot can get injured and this leads to foot ulcers.
B) Link to patient details:
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
History:- Patient has giddiness 7 days back and associated with 1 episode of vomiting on the same day.
•Patient was asymptomatic for 3 days, after which he consumed a small amount of alcohol He then developed giddiness, that was sudden in onset, continuous and gradually progressive.
•This was associated with Bilateral Hearing loss, aural fullness and presence of tinnitus.
•He has associated vomiting- 2-3 episodes per day, non projectile, non bilious containing food particles.
•Patient has H/o postural instability
Anatomical localization: cerebral vessels
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:
1)Tab Veratin 8 mg PO TID
Mechanism of action: Betahistine is one of the few drugs known which is said to improve the microcirculation of the inner ear. It works as a histamine analogue through 2 modes of action(1) agonist of H1 receptors and (2) antagonist of H3 receptors. It has a weak effect on H1 receptors but strong effect on H3 receptors.
2)Inj Zofer 4 mg IV/TID
Mechanism of action: Zofer Tablet works by inhibiting the action of a chemical substance named serotonin, which is responsible for inducing nausea and vomiting. Ondansetron binds to a receptor known as 5-HT₃, thus inhibits the binding of serotonin to it and prevents vomiting and nausea.
3)Tab Ecosprin 75 mg PO/OD
Mechanism of action: Ecosprin is an antiplatelet medicine. It works by inhibiting the action of an enzyme, which makes platelets aggregate together to form a blood clot.
4)Tab Atorvostatin 40 mg PO/HS
Mechanism of action: Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver.
5)BP monitoring- 4rth hourly
6)Tab Clopidogrel 75 mg PO/OD
Mechanism of action: The active metabolite of clopidogrelselectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible.
7)Inj Thiamine 1 AMP in 100 ml NSPO/BD
Mechanism of action: Thiamine combines with adenosine triphosphate (ATP) in the liver, kidneys, and leukocytes to produce thiaminediphosphate. Thiamine diphosphate acts as a coenzyme in carbohydrate metabolism, in transketolation reactions, and in the utilization of hexose in the hexose-monophosphate shunt.
8)Tab MVT PO/OD
3) Did the patients history of denovo HTN contribute to his current condition?
Answer:
Hypertension can cause stroke through many mechanisms. A high intraluminal pressure will lead to extensive alteration in endothelium and smooth muscle function in intracerebral arteries. The increased stress on the endothelium can increase permeability over the blood-brain barrier and local or multifocal brain oedema. Endothelial damage and altered blood cell-endothelium interaction can lead to local thrombi formation and ischaemic lesions.
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
C) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans: Evolution of symptoms :patient was normal 8 months back then developed b/l pedal edema which gradually progressed and Aggerevated in sitting and standing position, relived on taking medication
Palpitations :since 5days, sudden in onset which is more during night Aggerevated by lifting heavy weights, speaking continuously
Dyspnoea during palpitations (NYHA-3) since 5 days
pain:since 6days, radiating along left upper limb, more during palpitations and relived on medication.
Chest pain associated with chest heaviness since 5 days
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
Reason: recurrent hypokalemic periodic paralysis
Current risk factor:may be due to use of diuretics
Other risk factors
• Abnormal loses:
Medications-diuretics, laxatives, enema, corticosteriods
Real causes- osmotic diuresis, mineralo corticoid excess, renal tubular acidosis, hypomagnesenemia
• trance cellular shift : alkalosis, thyrotoxicosis, delirium tremans, head injury, Myocardial, ischemia, recurrent hypokalemic periodic paralysis
C) Inadequate intake: anorexia, dementia, stareation, total parental nutrition
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
D) Link to patient details:
QUESTIONS:
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
Ans:
A stroke causes your brain to become injured. The injury to your brain results in the formation of scar tissue, which affects the electrical activity in your brain. Disrupting the electrical activity can cause you to have a seizure.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Ans: It is may be due any scar formation or any hemorrhages which shows more severity in the symptoms.so, there is loss of consciousness in the recent attack
E) Link to patient details:
Questions: 1) What could have been the reason for this patient to develop ataxia in the past 1 year?
Ans:
• Damage from alcohol is a common cause of cerebellar ataxia. In patients with alcohol related ataxia, the symptoms affect gait (walking) and lower limbs more than arms and speech. It can also cause associated signs of peripheral neuropathy.
• Peripheral neuropathy is damage to the body's peripheral nervous system. This can cause muscle weakness, numbness and tingling, burning pain and a loss of coordination. This peripheral neuropathy, can contribute to the ataxia.
• Inside the brain, alcohol directly damages certain cells within the cerebellum and the rest of the brain, and for those people who drink excessively over a long period of time it can cause particularly severe and often permanent damage.
• Alcohol ataxia and other factors
Patients who drink excessively are often prone to nutritional deficiencies (e.g. thiamine, vitamin E) due to poor diet or damage to the gut lining, preventing the absorption of vitamins
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
Ans:
Heavy alcohol ingestion evidently exerts an inhibitory effect on platelet function even in the absence of alcohol in the blood, and this phenomenon is reversible on abstaining. The impaired platelet function, together with the reduced platelet count, may contribute to the bleeding diathesis associated with chronic alcoholism
F) Link to patient details:
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
Ans: yes
2.What are warning signs of CVA?•
• Sudden onset of weakness or numbness on one side of the body
•Sudden speech difficulty or confusion.
•Sudden difficulty seeing in one or both eyes.
•Sudden onset of dizziness, trouble walking or loss of balance.
•Sudden, severe headache with no known cause.
3.What is the drug rationale in CVA?
Answer:
1.Injection Mannitol 100ml/IV/TD
2.TAB Ecospirin 75 mg po/OD
3.TAB ATORVAS 40mg po/HS
4.BP/PR/TEMP/SP02 MONITORING (4th hourly)
5.RT FEEDS-100ml milk with protein powder(2nd hourly)
4. Does alcohol has any role in his attack?
Answer: Liver damage due to too much alcohol can stop the liver from making substances that help your blood to clot. This can increase your risk of having a stroke caused by bleeding in your brain.
5.Does his lipid profile has any role for his attack??
Answer:His HDL cholesterol levels are low
low serum HDL-C was associated with an increased risk of stroke.
G) Link to patient details:
__*Questions*_
1)What is myelopathy hand ?
Ans:
There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
2)What is finger escape ?
Ans:
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi. This finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign".
3)What is Hoffman’s reflex?
Ans:Hoffmann's reflex (Hoffmann's sign, sometimes simply "Hoffmann's", also finger flexor reflex) is a neurological examination finding elicited by a reflex test which can help verify the presence or absence of issues arising from the corticospinal tract.

H) Link to patient details:
Possible questions:
1) What can be the cause of her condition ?
Ans:
Seizures are the presenting feature of cerebral venous sinus thrombosis
2) What are the risk factors for cortical vein thrombosis?
Ans:
Risk factors for CVST:
• These include hormonal changes (e.g. oral contraceptives use, hormone replacement therapy, pregnancy and puerperium)
• mechanical precipitants (e.g. head trauma, jugular catheterization, surgery, lumbar puncture)
• local and generalized infections, cancer, acquired prothrombotic states (e.g. hyperhomocysteinemia, nephrotic syndrome)
• inflammatory diseases (e.g. vaculitis, intestinal inflammatory disease)
• hematological disorders
• neurological diseases (e.g. dural arteriovenous malformations, spontaneous intracranial hypotension), • drugs
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
Ans:
Reoccurance could be the persistence of excitable foci, till the oedema resolves.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Ans:
The drug used in suspicion of CVST are :
anticoagulants,Unfractionated heparin and low-molecular-weight heparin are most commonly used. Patients will also require long-term anticoagulation with an oral anticoagulant, such as warfarin
3) Cardiology (10 Marks)
A) Link to patient details:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
Heart failure with preserved ejection fraction occurs when the lower left chamber (left ventricle) is not able to fill properly with blood during the diastolic (filling) phase. The amount of blood pumped out to the body is less than normal. It is also called diastolic heart failure.
Heart failure with reduced ejection fraction happens when the muscle of the left ventricle is not pumping as well as normal. The ejection fraction is 40% or less. The amount of blood being pumped out of the heart is less than the body needs.
2.Why haven't we done pericardiocenetis in this pateint?
Ans:
Pericardiocentesis is indicated to remove fluid from the pericardial sac that surrounds the myocardium it is often performed in the settings of pericardial tampon add to correct the hypotension caused by decreased stroke volume,which is a result of the extrinsic compression of chambers of heart by pericardial fluid Here the pericardiocentesis is not done because of no cardiac tamponade
• 2.07cms effusion at the time of admission -1.4mm at the time of discharge)
• It's resolving so no need of invasive procedure when we are able to do conservatively
3.What are the risk factors for development of heart failure in the patient?
Ans:
Risk factors: in this patient
• Old age
• Smoking
• Alcohol
4.What could be the cause for hypotension in this patient?
May be some restriction due to pericardial effusion but not soo mch tht the functioning is impaired and leads to decreased venous return soo decreased cardiac output and hence hypotension
B) Link to patient details:
Questions:
1.What are the possible causes for heart failure in this patient?
Ans:
• patient has diabetes since 30yrs back and also having diabetic triopathy(neuropathy-retinopathy - nephropathy), so there is an increased risk for heart failure
• Hypertension since 19yrs - important risk factor
• Chronic alcoholic since 40yrs, leads to decreased LVEFand causes LV dysfunction
• patient has elevated creatinine, chronic kidney disease, AST/ALT greater than 2,all of this are important risk factors for heart failure
2.what is the reason for anaemia in this case?
Ans:
• Alcoholism: Alcoholism impact RBC production as it decreases the no of precursor cells in the marrow resulting in fewer mature RBCs and anemia
• kidney disease leads to decreased function of kidney leading to decreased erythropoietin synthesis and leads to anemia
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
Ans :
• Patient being diabetic which leads to imparting the healing process leading to non healing ulcers
• Alcoholism also leads to poor wound healing
4. What sequence of stages of diabetes has been noted in this patient?
• The patient was diagnosed by diabetes 30years ago • Since 4 years :
he had blurring of vision ( diabetic retinopathy)
He had CKD ( diabetic nephropathy)
• He also had non healing ulcers
C) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
- Patient was apparently asymptomatic 2 days ago when he developed Shortness of breath Grade II (on exertion) which progressed to Grade IV (at rest) for which he visited local RMP and was referred to our hospital.
- Patient also complains of decreased urine output since 2 days and Anuria since morning.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans:
• INJ. Dobutamine 3.6ml/hr was given to maintain the falling BP up to a MAP of 55 mmHg
Mechanism of action:
Dobutamine is a synthetic catecholamine that acts on alpha-1, beta-1 and beta-2 adrenergic receptors. In the heart, the stimulation of these receptors produces a relatively strong, additive inotropic effect and a relatively weak chronotropic effect.
• ECG showed Irregular rhythm and he was started on TAB. Digoxin 0.25mg OD 5/7 and INJ. Unfractionated Heparin 5000 IU TID.
Mechanism of action of digoxin:
• Patient was started on TAB. Carvediol 3.125mg BD
Mechanism of action:
Carvedilol reversibly binds to beta adrenergic receptors on cardiac myocytes. Inhibition of these receptors prevents a response to the sympathetic nervous system, leading to decreased heart rate and contractility.
• Patient was started on INJ. Unfractionated Heparin Infusion @5ml/hr and TAB. Acetyl cysteine 600mg PO TID.
Mechanism of action: NAC is a precursor of glutathione, it increases the concentration of glutathione available for the conjugation of NAPQI. NAC also enhances sulfate conjugation of unmetabolized APAP, functions as an anti-inflammatory and antioxidant, and has positive inotropic effects.
• TAB. Acitrom 2mg OD
Other medications used during the course in hospital - 1. TAB. Cardivas3.125mg PO/BD
2. TAB. Dytor 10mg PO/OD
Indication: and is used to treat high blood pressure and condition of excess fluid retention in the body due to heart failure, kidney or liver diseases.
3. TAB Pan D 40mg PO/OD
4. TAB. Taxim 200mg PO/OD
Mechanism of action: it inhibits the Na-K-2Cl channel
5. INJ. Thiamine 100mg in 50ml NS IV/TID
6. INJ. HAI S.C 8U-8U-6U
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
This patient has cardio renal syndrome 2
4) What are the risk factors for atherosclerosis in this patient?
Answer:
High cholesterol and triglyceride levels.
High blood pressure.
Smoking.
Type 1 diabetes.
Obesity.
Physical inactivity.
High saturated fat diet.
5) Why was the patient asked to get those APTT, INR tests for review?
Answer: Standard coagulation screening tests such as activated partial thromboplastin time (APTT), prothrombin time (PT), and the international normalized ratio (INR) are important constituents of basic examinations in clinical laboratories. APTT can be used as an indicator of intrinsic coagulation pathway activity, and a short APTT is linked to increased thrombin generation and increased risk for thrombosis.
D) Link to patient details:
67 year old patient with acute coronary syndrome
https://daddalavineeshachowdary.blogspot.com/2021/05/67-year-old-patient-with-acute-coronary.html?m=1
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer: History:- She had H/O heartburn like episodes since a year. They were relived without use of any medication.
She has H/O TB diagnosed 7 months ago for which she completed the course of medication a month ago.
shortness of breath (SOB) since 1/2 hour.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer: TAB MET XL 25 MG/STAT.
Mechanism of action: Met XL 50 Tablet works by blocking the effects of some chemicals on your heart and blood vessels. It slows down your heart rate and helps it to beat with less force.
3) What are the indications and contraindications for PCI?
Answer: Clinical indications for PCI include the following:
Acute ST-elevation myocardial infarction (STEMI)
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Unstable angina.
Stable angina.
Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
High risk stress test findings.
Contraindications to Percutaneous Coronary Interventions
Lack of cardiac surgical support.
Critical left main coronary stenosis without collateral flow from a native vessel or previous bypass graft to the left anterior descending artery.
Coagulopathy.
Hypercoagulable states.
Diffusely diseased vessels without focal stenoses.
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
Answer: Medical therapy with high dose statins is preferred over balloon angioplasty in patients with mild anginal symptoms.
PCI is preferred over medical therapy has:
1) severe symptoms
2) failed medical therapy
3) high risk coronary anatomy
4) worsening LV function
OVERTREATMENT: The main and worst consequences of overdiagnosis is overtreatment if an incident lesion or disease which is unlikely to have benefits for the patient. At the same time the likely interventions like surgery, radiation and chemotherapy can have side effects resulting in significant morbidity and fatalities can occur. As over diagnosis is some non neoplastic conditions leads to over prescription and over medicalisation , and resulting in many undesirable and sometimes dangerous side effects.
E) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
a)patient came with the symptoms of chest pain 3 dys back, giddiness and profuse sweating since morning
Patient is suffering from right side chest pain from 3 dys (insidious progressive and dragging type which is radiating to back) and also patient developed giddiness along with sweating since morning
ANATOMICAL LOCATION :inferior wall mi
PRIMARY ETIOLOGY :patient is a known case of type 2 diabetes mellitus since 8 years and hypertension
Since patient is a diabetic he developed high glucose levels which in turn leads to high cholesterol levels(HYPERCHOLESTREMIA) . High cholesterol and hypertension are the major risk factors fr the development of myocardial infarction
Hyper cholesteremia leads to fat and cholesterol accumulation in the walls of arteries leading to blockage of artery which in turn leads to MI. So diabetes and hypertension both are the major causes for the development of myocardial infarction in this patient
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
2.Mechanisam of action :
1)Aspirin : It is an antiplatelet drug. It acts by inhibiting thromboxane synthesis thus inhibits platelets aggregation. It reduces the risk of progression to MI and sudden death.
2)Atorvas: They are hypolipidaemic drugs. They act by inhibiting HMG-CoA reductase enzyme. This results in compensatary increase in LDL receptors in liver cells and causes increased receptor meditated uptake and catabolism of IDL and LDL. They are first choice of drugs for dyslipidemia in diabetics.
3)Clopibb: It is also a antiplatelet drug. Acts by inhibiting the P2Y 12 receptor on the surface of platelets. Combination of aspirin and clopidogrel is synergistic in preventing ischemic episodes.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
3.Yes PTCA is protective and is needed for good prognosis. It prevents recurrence of MI attack
4) Gastroenterology (& Pulmonology) 10 Marks
A) Link to patient details:
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A)Acute Pancreatitis:-
1.Symptomatology:- Pain in abdomen since 1wk
Vomiting since 1wk
Fever since 4 daya
Constipation since 4daya
Burning micturition since 4days
Anatomical localisation:-
The pancreas lies behind the peritoneum of the posterior abdominal wall and is oblique in its orientation. The head of the pancreas is on the right side and lies within the “C” curve of the duodenum at the second vertebral level (L2)
Primary etiology:- Alcoholism
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
1. ING. MEROPENAM ; TID for 7 days
Mechanism of action:
Meropenem is bactericidal except against Listeria monocytogenes, where it is bacteriostatic. It inhibits bacterial cell wall synthesis like other β-lactam antibiotics. In contrast to other beta-lactams, it is highly resistant to degradation by β-lactamases or cephalosporinases.
2 .ING. METROGYL 500 mg IV TID for 5 days
Mechanism of action :
Metronidazole diffuses into the organism, inhibits protein synthesis by interacting with DNA and causing a loss of helical DNA structure and strand breakage. Therefore, it causes cell death in susceptible organisms.
3. ING. AMIKACIN 500 mg IV BD for 5days
4. TPN ( Total Parenteral Nutrition )
5.IV NS / RL at the rate 12l ml per hour
6. ING. OCTREOTIDE 100 mg SC , BD
Octreotide binds to somatostatin receptors coupled to phospholipase C through G proteins and leads to smooth muscle contraction in the blood vessels.Downstream effects that stimulate phospholipase C, the production of 1, 4,5-inositol triphosphate, and action on the L-type calcium channels lead to the inhibition of growth hormone, treating the various growth-hormone and metabolic effects of acromegaly.
Octreotide's suppression of luteinizing hormone (LH) reduction in splanchnic blood flow and inhibition of serotonin, gastrin, vasoactive intestinal peptide, secretin, motilin, and pancreatic polypeptide provide relief for the gastrointestinal and flushing symptoms of carcinoid and/or VIPoma tumors.
7.ING. PANTOP 40 mg IV , OD
8. ING. THIAMINE 100 mg in 100 ml NS IV , TID
9. ING. TRAMADOL in 100 ml NS IV , OD
Mechanism of action:
Tramadol is a centrally acting analgesic with a multimode of action. It acts on serotonergic and noradrenergic nociception, while its metabolite O-desmethyltramadol acts on the µ-opioid receptor
The pseudocyst was drained per cutaneously per abdominally under local anaesthesia with USG guided malecot drain placed inside and pus was drained.
Oxygen supply for mild hypoxia , which was
developed due to pneumothorax ( Spo2: 98% on 6 lts of oxygen )
ICD ( Inter Coastal Drainage ) placed for pneumothorax.
B) Link to patient details:
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
Ans:
Acute pancreatitis in its severe form is complicated by multiple organ system dysfunction, most importantly by pulmonary complications which include hypoxia, acute respiratory distress syndrome, atelectasis, and pleural effusion. The pathogenesis of some of the above complications is attributed to the production of noxious cytokines. or may be due to Hepatic hydrothorax in which Abdominal fluid fills the lung (mostly on the right side) and causes SOB
2) Name possible reasons why the patient has developed a state of hyperglycemia.
Ans:
The pathogenesis of pancreatogenic diabetes is mainly explained by the development and progression of destructive changes, hypoxic changes in devitalized pancreatic tissues, and endocrine sclerosis.
It is result of primary inflammation of the pancreatic paren-
chyma in ACP which has a linear dependence on the frequency and duration of the disease, and the likelihood of developing diabetes with an exacerbation of the process
during 5-8 years is 17.5%
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
Ans:
In general, ALD should be suspected in patients with a significant history of alcohol use who present with abnormal serum transaminases, particularly if the level of aspartate aminotransferase (AST) is greater than that of alanine aminotransferase (ALT), hepatomegaly, clinical signs of chronic liver disease, radiographic evidence of hepatic steatosis or fibrosis/cirrhosis, or who have had a liver biopsy showing macrovesicular steatosis or cirrhosis. Patients with ALD may or may not have elevated serum aminotransferase levels. The absolute level of liver enzyme elevation does not correlate well with the severity of ALD, however, the pattern of elevation in
transaminases is helpful in making a diagnosis of liver injury due to alcohol as AST is typically two to three times greater than ALT in alcoholic liver injury. They will also typically have an elevated serum gamma glutamyltranspeptidase (GGT). However, it is important to rule out other etiologies for the patient's liver disease before making a definitive diagnosis of ALD, including chronic viral hepatitis, autoimmune hepatitis, hemochromatosis and drug related hepatotoxicity. In some cases, when the diagnosis is unclear, a liver biopsy may be warranted.
4) What is the line of treatment in this patient?
Ans:
Treatment includes a combination of goal-directed fluid therapy, pain control( morphine), antiemetics, electrolyte replacement, early enteral nutrition, alcohol cessation counseling and diuretics for ascites
IC) Link to patient details:
Possible Questions :-
1) what is the most probable diagnosis in this patient?
Ans: Ruptured liver abcess
Grade 3 RPD in right kidney
2) What was the cause of her death?
Ans: Her cause of death might be due to sepsis
3) Does her NSAID abuse have something to do with her condition? How?
Ans:she had grade-3 RPD changes in right kidney
She may be having underlying CKD which is secondary to her NSAID abuse (Analgesic nephropathy)
5) Nephrology (and Urology)
A) Link to patient details:
1.what could be the cause for his SOB
Ans- His sob is due to Acidosis which was caused by Diuretics
2. Reason for Intermittent Episodes of drowsiness
Ans-Hyponatremia was the cause for his drowsiness
3.why did he complaint of fleshy mass like passage inurine
Ans-plenty of pus cells in his urine passage appeared as
fleshy mass like passage to him
4. What are the complicat ions of TURP that he may have had
Ans-
Difficulty micturition
Electrolyte imbalances
Infection
B) Link to patient details:
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?
This might be because of :
There is no association with
Flank pain
Lower abdominal pain
Burning sensation while micturating
Fever
Malaise
2. Why doesn't the child have the excessive urge of urination at night time ?
Ans: Since the child does not get the urgency to urinate when he is asleep, there can be a chance of the manifestation being psychosomatic, or as a result of an undiagnosed anxiety disorder , or a stressor triggering this manifestation.
3. How would you want to manage the patient to relieve him of his symptoms?
Ans: The child need counselling sand therapies
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology)
A) Link to patient details:
Questions:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
Ans: history findings:
• Coughing when feeding
Physical findings:
• laryngeal crepitus
• On CECT of thorax: fistula is communication between left main bronchus and mid thoracic esophagus few centimetres below carina
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
Immune reconstitution inflammatory syndrome(IRIS) is a condition seen in some cases of AIDS or immunosuppression, in which the immune systembegins to recover, but then responds to a previously acquired opportunistic infection with an overwhelming inflammatory response that paradoxically makes the symptoms of infection worse. In this case the patient was HIV positive from 2012 and recently got TB positive which can lead to IRIS
How can immune reconstitution inflammatory syndrome be prevented? The most effective prevention of IRIS would involve initiation of ART before the development of advanced immunosuppression. IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-cell count greater than 100 cells/uL.
7) Infectious disease and Hepatology:
Link to patient details:
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors
present in it ?
Ans: alcoholism, mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver. It is also proven that Alcoholism is never an etiological factor
What could be the cause in this patient ?
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
3. Is liver abscess more common in right lobe ?
Ans:
liver abscesses occur in the right lobe of the liver (a more significant part with more blood supply), less commonly in the left liver lobe
4.What are the indications for ultrasound guided aspiration of liver abscess ?
Ans:• Feature of impending rupture or compression sign
• size > 6cm
• multiple abscesses involving both right and left lobes
• Failure in the improvement or aggravation on conservative treatment even after 72 hrs
B) Link to patient details:LIVER ABSCESS
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-liver-abcess.html
QUESTIONS:
1) Cause of liver abcess in this patient ?
Answer: Amoebic liver abscess (ALA) is the most common manifestation of invasive amoebiasis caused by Entamoeba histolytica (EH). Several studies from India have reported a strong link between consumption of toddy and the occurrences of ALA. Toddy is a local alcoholic beverage consisting of fermented palm juice.
2) How do you approach this patient ?
Answer: Based on right hypochondriac and epigastric pain , fever and USG findings
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
Considering the age of patient young and male and single abcess in the right lobe the the abcess is more likely to be a amoebic
Since we cannot take risk , we should however administer antibiotics also ( like in pyogenic liver abcess)
Answer: Amoebic liver abscess: The first line treatment in uncomplicated amebic abscess should be amebicidial drugs. Metronidazole is the drug of choice and has replaced the use of emetine and chloroquine. Metronidazole is effective against both the intestinal and hepatic phase. 750 mg three times a day for 7–10 days is recommended.
Payogenic liver abscess: Treatment usually consists of placing a tube through the skin into the liver to drain the abscess. Less often, surgery is needed. You will also receive antibiotics for about 4 to 6 weeks. Sometimes, antibiotics alone can cure the infection.
4) Is there a way to confirmthe definitive diagnosis in this patient?
Answer: Analysis of reports and diagnosis:
*Based on right hypochondriac and epigastric pain , fever
* USG finding of hyperechoic mass in right lobe of liver along with other supportive investigations like leucocytosis ( suggestive of infection/inflammation) and ALP ( Alkaline phosphatase ) rise in LFT is a suggestive diagnosis of LIVER ABCESS.
* Considering the following factors:
1) Age of the patient (21) - young & gender- male
2) Single abcess,
3) Right lobe involvement,
# The abcess is most likely to be AMOEBIC LIVERABCESS.
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology) 10 Marks
A) Link to patient details:
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans:
18/04/21 He went to local PHC for COVID 19 vaccination.. Since that night patient is complaining of Fever associated with chills and rigors, high grade fever, no diurnal variation which was relieved on medication...
No c/o cold and cough
Followed by patient is having similar complaints after three days and he visited local hospital which is not subsided by medication ( Antipyretics) ( not taken medication such as steroids, oxygen therapy, anti virals)
On 28/04/21 , c/o Generalized weakness and facial puffiness and periorbital edema.. And also patient is in drowsy state..
On 04/05/21, patient presented to casualty In altered state with facial puffiness and periorbital edema and weakness of right upper limb and lower limb...
primary etiology: Diabetes can lead to mucormycosis
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Proposed management -
Inj. Liposomal amphotericin B according to creatinine clearence
Loading dose 30mg/IV over 2-6 hrs
Maintenance dose 60mg / IV once a day
Treatment modalities:
The successful treatment of mucormycosis requires four steps: 1) early diagnosis; 2) reversal of underlying predisposing risk factors, if possible; 3) surgical debridement where applicable; and 4) prompt antifungal therapy [3].
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
Thus far, this surge has been attributed to the improper use of steroids to treat Covid-19 patients, coupled with poorly managed diabetes. But steroids in themselves are not the villains.
“Systemic (oral and intravenous) corticosteroids have been proven to reduce mortality in Covid-19, “The largest trial, Recovery, which proved this beyond a reasonable doubt among individuals who had low oxygen levels, used them in a dose of 6 milligrams Dexa per day for up to 10 days.”
Not only in Covid-19, but steroids are also widely used in orthopaedic and pulmonary diseases. In India, the problem lies not in the drug but in how it is prescribed. “Most of us who work in India will agree that prescribing practices more often than not tend towards higher doses for longer periods of time, which is a clear risk factor for invasive fungal infections
Medicines used in treating Covid-19 tend to bring down the count of lymphocytes. Lymphocytes are one of the three types of white blood cells whose job is to defend our body against disease-causing pathogens such as bacteria, viruses, and parasites. The reduced count of lymphocytes leads to a medical condition called lymphopenia, making way for opportunistic fungal infection in Covid-19 patients.
There is a higher chance of occurrence of mucormycosis in patients whose immune system is not functioning well, and since Covid-19 treatment tends to suppress the working of the immune system, it places such patients at a higher risk of contracting the black fungus infection.


























Comments
Post a Comment