23 CH AKHILA
A 65 YEAR OLD FEMALE
ON 11/9/21
1.Salt restriction <2.4 gm/ day
2.INJ.PANTOP 40 MG/IV/OD
3.INJ.ZOFER 4 MG/IV/TID
4.TAB.DOLO 650 MG/PO/TID
5.INJ NEOMAL 100 ML IV/SOS
6.TAB ULTRACET /PO/QID
7.Syp.Ascoryl D 15 ml/po/tid
8.pr/bp/rr charting 2nd HRLY
9.I/O charting
ON 12/9/21
1.IVF -NS,RL@150 ML/HR
2.SALT RESTRICTION <2.4 GM/DAY
3.TAB.PANTOP 40 MG/PO/OD
4.INJ.ZOFER 4 MG/IV/TID
5.INJ NEOMAL 100 ML IV/SOS
6.TAB.DOLO 650 MG/PO/TID
7.TAB ULTRACET /PO/QID
8.Nebulisation with DUOLIN 6TH HRLY
And budecort 12 th HRLY
9.Syp.Ascoryl D 10 ml/po/tid
10.pr/bp/rr charting 2nd HRLY
11.I/O charting
12.GRBS -6TH HRLY
ON 13/9/21
Day 3
SUBJECTIVE-
Fever
Body pains
Generalized weakness
OBJECTIVE-
Temp-98.5 F
Pr-105bpm ,regular,bounding pulse
BP- 140/70MM HG
RS-BAE+ , decreased air entry b/l IAA,ISA,Wheeze +
Rr-24cpm
Spo2-93% @RA
CVS-S1,S2 heard
P/A- soft
GRBs-109 mg/dl
Stools-not passed
ASSESSMENT-
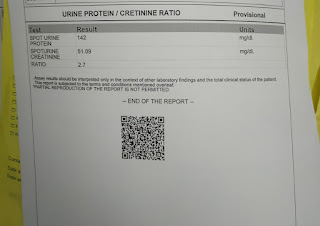
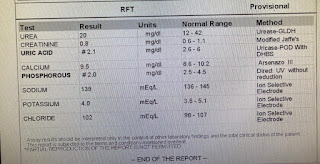
?UTI With Pre renal AKI
?chronic bronchitis
Paroxysmal AF(resolved)
PLAN OF TREATMENT-
1.IVF -NS,RL@100 ML/HR
2.O2 inhalation -4 lit to maintain spo2
3.Inj.ZOSTUM 1.5 gm/iv/bd
4.TAB.PANTOP 40 MG/PO/OD
5.INJ.ZOFER 4 MG/IV/TID
6.TAB.DOLO 650 MG/PO/TID
7.TAB ULTRACET /PO/QID
8.Nebulisation with ipravent 6TH HRLY
And budecort 12 th HRLY
9.Syp.Ascoryl D 10 ml/po/tid
10.pr/bp/rr charting 2nd HRLY
11.I/O charting
On 14/9/21
A 65 year old female
Subjective:
1 episode of vomiting at 4 am today
Fever spikes from 8am to 2pm yesterday, no fever episodes thereafter
OBJECTIVE-
Temp-98.5 F
Pr-78bpm ,regular,bounding pulse
BP- 120/70MM HG
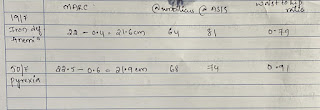
RS-BAE+ , decreased air entry b/l IAA,ISA
Left iAA,ISA inspiratory crepts+
Rr-24cpm
Spo2-95% @RA
CVS-S1,S2 heard
P/A- soft
GRBs-109 mg/dl
Stools- passed
ASSESSMENT-
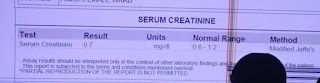
Her creatinine has come down 2.8mg/dl to 1.1mg/dl
Acute GE with Pre renal AKI
?acure bronchitis
Paroxysmal AF(resolved)
PLAN OF TREATMENT-
1.IVF -NS,RL@100 ML/HR
2.O2 inhalation
3. Day 2 of Inj Piptaz 2.5gm gm/iv/TID
Inj Metrogyl 400mg/IV TID
4.TAB.PANTOP 40 MG/PO/OD
5.INJ.ZOFER 4 MG/IV/TID
6.TAB.DOLO 650 MG/PO/TID
7.TAB ULTRACET half tab /PO/QID
8.Nebulisation with ipravent 6TH HRLY
And budecort 12 th HRLY
9.Syp.Ascoryl D 10 ml/po/tid
10.pr/bp/rr charting 2nd HRLY
11.I/O charting
On16/9/21
SOAP NOTES
Subjective:
Generalized weakness
No fever spikes
Cough (reduced)
OBJECTIVE-
Temp-98.3F
Pr-80bpm ,regular,bounding pulse
BP- 140/80MM HG
RS-BAE+ , decreased air entry b/l IAA,ISA
Left iAA,ISA inspiratory crepts+
Rr-20cpm
CVS-S1,S2 heard
P/A- soft
Stools- not passed
ASSESSMENT-
? acute bronchitis
Paroxysmal AF(resolved)
Pre renal AKI SECONDARY TO acute GE
DENOVO HTN
PLAN OF TREATMENT-
1.IVF -NS,RL@100 ML/HR
2.O2 inhalation
3.TAB.PANTOP 40 MG/PO/OD
4.INJ.ZOFER 4 MG/IV/TID
5.TAB.DOLO 650 MG/PO/TID
6.TAB ULTRACET half tab /PO/QID
7.Nebulisation with ipravent 6TH HRLY
And budecort 12 th HRLY
8.Syp.Ascoryl D 10 ml/po/tid
9.pr/bp/rr charting 2nd HRLY
10.I/O charting
On 17/9/21
SOAP NOTES
Ward case
A 65 year old female
Subjective:
No fever spikes
Cough (reduced)
OBJECTIVE-
Temp-98.3F
Pr-84bpm ,regular,bounding pulse
BP- 140/80MM HG
RS-BAE+ , decreased air entry b/l IAA,ISA
Left iAA,ISA inspiratory crepts+
Rr-20cpm
CVS-S1,S2 heard
P/A- soft
Stools- passed
ASSESSMENT-
? acute bronchitis
Paroxysmal AF(resolved)
Pre renal AKI SECONDARY TO acute GE
DENOVO HTN
PLAN OF TREATMENT-
1.IVF -NS,RL@100 ML/HR
2.O2 inhalation
3.TAB.PANTOP 40 MG/PO/OD
4.INJ.ZOFER 4 MG/IV/TID
5.TAB.DOLO 650 MG/PO/TID
6.TAB ULTRACET half tab /PO/QID
7.Nebulisation with ipravent 6TH HRLY
And budecort 12 th HRLY
8.Syp.Ascoryl D 10 ml/po/tid
9.pr/bp/rr charting 2nd HRLY
10.I/O charting.

























Comments
Post a Comment