Final practical short case
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
45 Y/O female with fever and rash
A 45-year-old female tailor by occupation came to the hospital with chief complaints of fever on and off, associated with generalized body pains, loss of appetite for 3 months, facial rash since 10days.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 10 years back then she developed joint pains started first in the knees and ankles then slowly progressed to hands associated with swelling and morning stiffness for 10 min,and for this patient went to a private hospital and found RA factor positive and treated with diclifenac and patient was asymptomatic for 8 months
Appetite- decreased
Bowel and bladder- regular
Sleep- disturbed
Addictions- nil
GENERAL EXAMINATION :
Patient is conscious coherent cooperative and well-oriented with time, place, and person
moderately built and nourished
Pallor - Present
No icterus, clubbing, cyanosis, lymphadenopathy, and edema
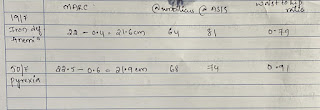
VITALS:
Patient was afebrile
BP: 110/70 mmhg,
PR: 78bpm,
RR:18 cpm
SP02: 98%
LOCAL EXAMINATION:
Swelling at ankle associated with redness and local rise of temperature and itching pigmentation and pain which is throbbing type non radiating no aggravating and relieving factors and dorsalis pedis pulses were felt
The erythematous rash is present on the face which is not associated with the itching but was there 10days back gradually subsided
SYSTEMIC EXAMINATION;
CVS:
inspection shows no scars on the chest, no raised JVP, no additional visible pulsations seen
all inspectory findings are confirmed
apex beat normal at 5th ics medial to mcl
no additional palpable pulsations or murmurs
percussion showed normal heart borders
auscultation S1 S2 heard no murmurs
MOTOR-: normal tone and power
reflexes: RT LT
BICEPS ++ ++
TRICEPS ++ ++
SUPINATOR ++ ++
KNEE ++ ++
SENSORY :
touch, pressure, vibration, and proprioception are normal in all limbs
GIT:
inspection- normal scaphoid abdomen with no pulsations and scars
palpation - inspectory findings are confirmed
no organomegaly, non tender and soft
percussion- normal resonant note present, liver border normal
auscultation-normal abdominal sounds heard, no bruit present
RESPIRATORY:
inspection: normal chest shape bilaterally symmetrical, mediastinum central
no scars, Rr normal, no pulsations
palpation: Insp findings are confirmed
percussion: normal resonant note present bilaterally
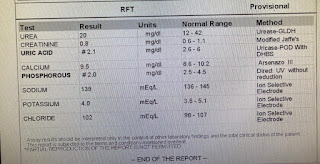
Investigations:
PROVISIONAL DIAGNOSIS:
Secondary sjogren syndrome
Anaemia secondary to chronic inflammatory disease
with LT LL cellulitis
B/L Optic atrophy








Comments
Post a Comment