Final Practical Long case
1701006032 CASE PRESENTATION
LONG CASE :
A 30 year old female patient who is house wife by occupation resident of Nalgonda came to OPD with chief complaints of
Chief complaints :
Facial puffiness and pedal Edema since 2 days
Shortness of breath since 2 days
Abdominal pain since 2days
History of presenting illness :
Patient was asymptomatic 7 months back and she developed facial puffiness and bilateral leg swelling which was pitting in type
SOB: insidious in onset gradually progressed to grade 4 not associated with change in position no aggravating and relieving factors
Abdominal pain : pain in epigastric region
since 2days which was started suddenly and burning type of pain
Past history
She is a known case of hypertension since 12 years
Personal history :
Appetite : decreased
Diet : mixed
Sleep : inadequate
Bladder : decreased urine output
Bowel movements: normal
Addictions :absent
Family history:
Patients mother is hypertensive
General examination:
Pallor: present
Icterus: absent
Cyanosis : absent
Clubbing : absent
Lymphadenopathy : absent
Edema : absent
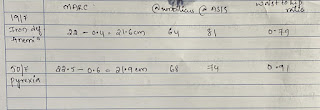
Vitals:
Temperature: a febrile
Pulse: 120 bpm
Blood pressure: 150/90mmHg
Respiratory rate : 34 cpm
Systemic examination:
Respiratory system:
Patient examined in sitting position
Inspection:-
oral cavity- Normal ,nose- normal ,pharynx-normal
Respiratory movements : bilaterally symmetrical
Trachea is central in position & Nipples are in 4th Intercoastal space
Apex impulse is not visible
Palpation:-
All inspiratory findings are confirmed
Trachea central in position
Apical impulse in left 6th ICS, slightly lateral
Respiratory movements bilaterally symmetrical
Tactile and vocal fremitus reduced on both sides in infra axillary and infra scapular region , mammary regions
PERCUSSION
DULL IN BOTH SIDES
AUSCULTATION :
DECREASED BREATH SOUNDS ON BOTH SIDES
Cardiovascular system
JVP -raised
Visible pulsations: absent
Apical impulse : shifted downward and laterally
Thrills -absent
S1, S2 - heart sounds muffled
Pericardial rub -present
Abdomen examination:
INSPECTION
Shape : distended
Umbilicus:normal
Movements :normal
Visible pulsations :absent
Skin or surface of the abdomen : normal
PALPATION
Liver is not palpable
PERCUSSION : Dull
AUSCULTATION :bowel sounds heared
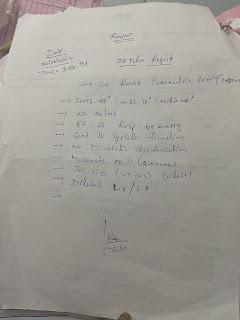
Chest x-ray:
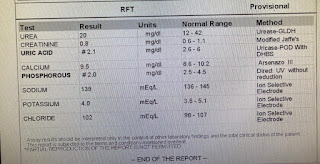
PROVISIONAL DIAGNOSIS:
Chronic kidney disease on maintainance hemodialysis
Ascites
Treatment:
INJ. MONOCEF 1gm/IV/BD
INJ. METROGYL 100ml/IV/TID
INJ PAN 40mg/IV/OD
INJ. ZOFER 4mg/iv/SOS
TAB. LASIX 40mg/PO/BD
TAB. NICORANDIL 20mg/PO/TID
INJ. BUSOCOPAN /iv/stat
Add on
TAB. OROFENPO/BD
TAB. NODOSIS 500mg/PO/TID
INJ.EPO 4000 ml/ weekly
TAB. SHELLCAL/PO/BD
DIALYSIS (HD)
INJ.KCL 2AMP IN 500 ml NS over 5min
























Comments
Post a Comment